Real-Time Insurance Verification for Healthcare
Pod instantly verifies patient insurance coverage and eligibility by phone—connecting with your EMR, EHR, or billing system. Reduce manual checks, cut wait times, and give patients answers in seconds, not days.

Connect with Every Major Insurance & Healthcare System
Pod integrates with national and local payors, clearinghouses, EMR/EHR systems, and healthcare billing software. Automate verification, eligibility checks, and insurance updates with a single platform.
Find the software you useAirtable
Buffer
Cal.com
Calendly
Close
Cognito Forms
Customer.io
Docusign
Eventbrite
Gmail
Google Ads
Google Analytics 4
Google BigQuery
Google Calendar
Google Contacts
Google Docs
Google Drive
Google Forms
Google Sheets
Granola
HubSpot
Jotform
LinkedIn Ads
LinkedIn Conversions
Mailchimp
Microsoft Excel
Microsoft Office 365
Microsoft Outlook
Motion
MySQL
Notion
PayPal
Pipedrive
SEMrush
SQL Server
Salesforce
SendGrid
Square
Stripe
Tally
Telegram
Telnyx
Textline
Trello
Twilio
Typeform
WooCommerce
Zendesk
Zoho CRM
Zoho Recruit
Airtable
Buffer
Cal.com
Calendly
Close
Cognito Forms
Customer.io
Docusign
Eventbrite
Gmail
Google Ads
Google Analytics 4
Google BigQuery
Google Calendar
Google Contacts
Google Docs
Google Drive
Google Forms
Google Sheets
Granola
HubSpot
Jotform
LinkedIn Ads
LinkedIn Conversions
Mailchimp
Microsoft Excel
Microsoft Office 365
Microsoft Outlook
Motion
MySQL
Notion
PayPal
Pipedrive
SEMrush
SQL Server
Salesforce
SendGrid
Square
Stripe
Tally
Telegram
Telnyx
Textline
Trello
Twilio
Typeform
WooCommerce
Zendesk
Zoho CRM
Zoho Recruit
Need a custom integration built? Let us handle it for you today.
Contact Sales
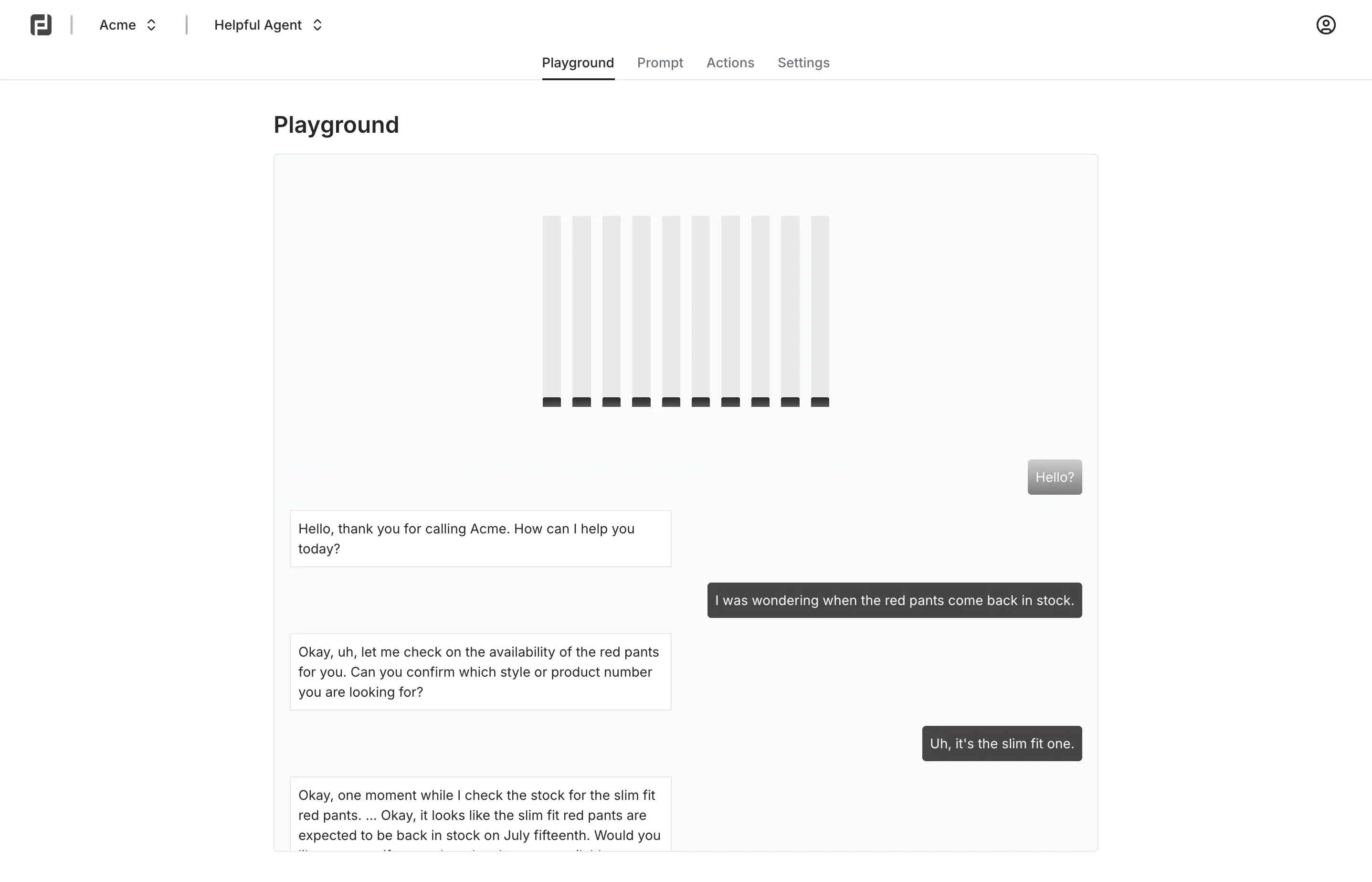
Verify Insurance in Seconds, Not Days
Patients and staff can check insurance eligibility or coverage by phone 24/7. Pod’s AI agent pulls real-time data from your systems and payors—no more hold times, voicemails, or paperwork.

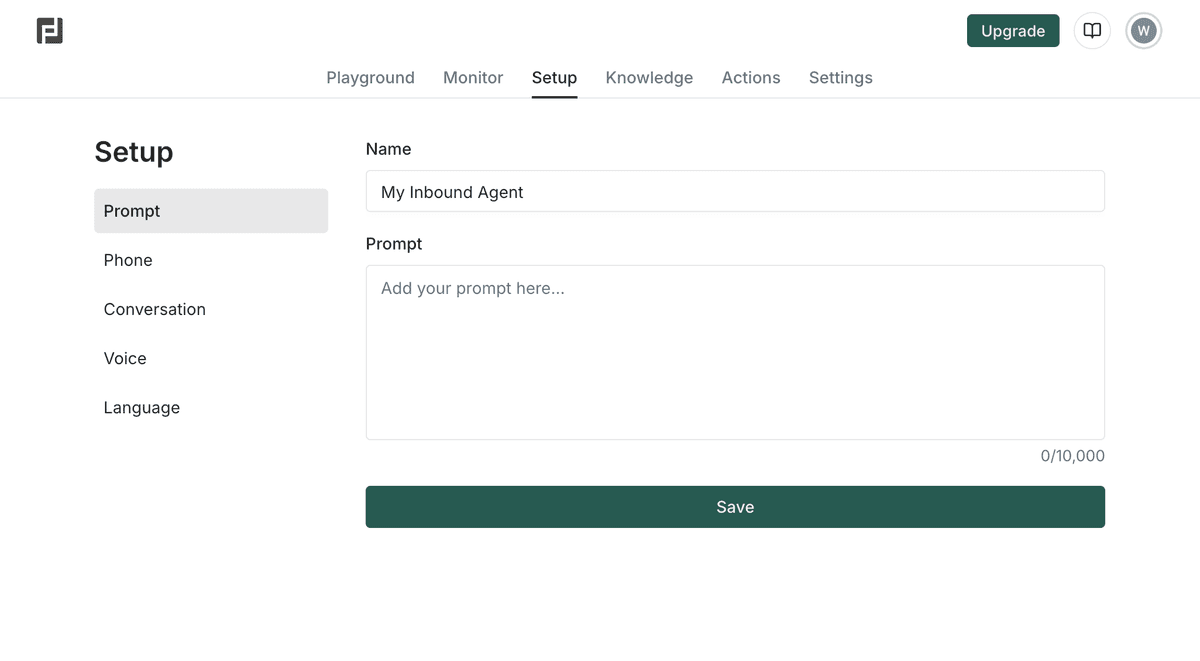
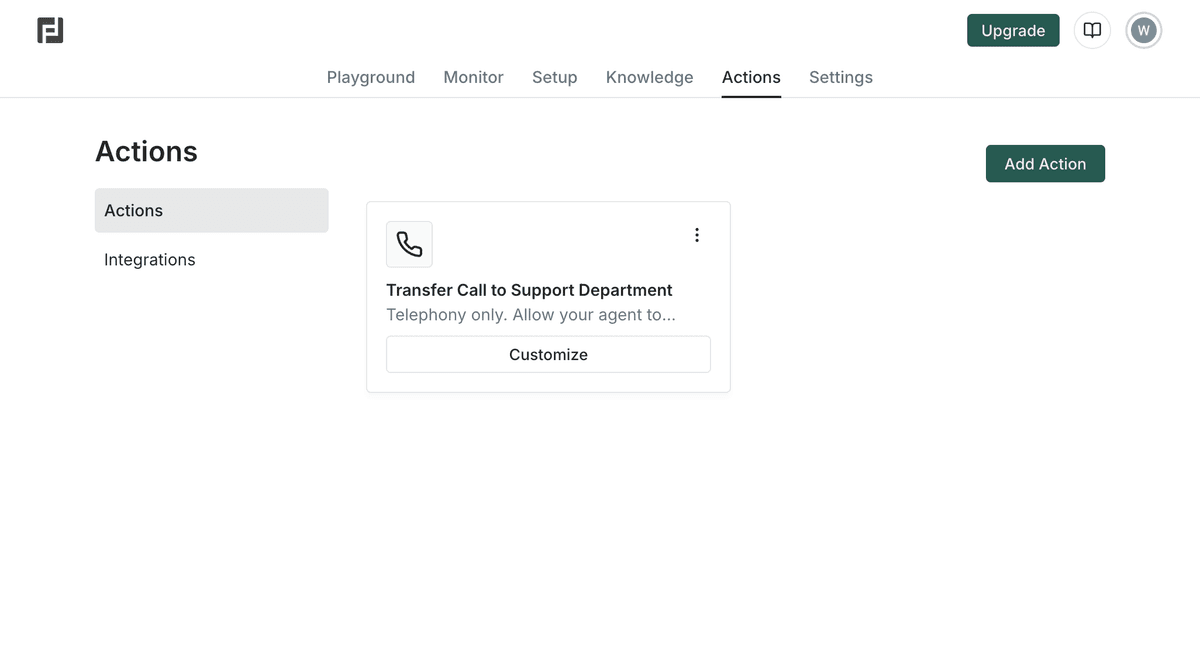
Automate Eligibility Checks & Pre-Visit Screening
Pod collects insurance details, runs eligibility checks, and notifies your team or the patient of coverage status before the visit. Reduce claim denials, billing headaches, and front desk workload.

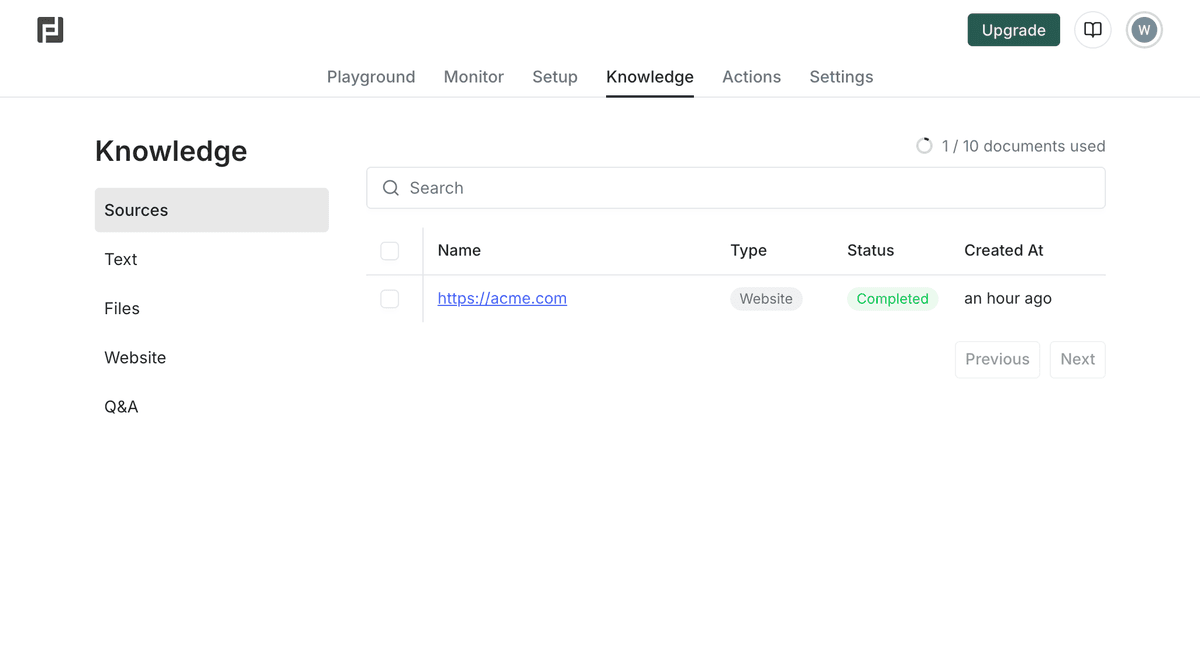
Seamless Integration with Your Healthcare Stack
Pod connects to leading EMR, EHR, and billing systems, as well as regional insurance databases and payors—ensuring compliance and accuracy for every insurance check.
AI Insurance Verification for Healthcare Providers
Let Pod verify coverage, check eligibility, and collect patient details over the phone—so your front desk can focus on care, not paperwork.

Instant insurance verification
Check patient coverage and eligibility with top insurers in real time, by phone or API.
Automated eligibility screening
Collect patient info, run payer checks, and get instant confirmation of coverage status.
Integration with EMR, EHR & billing
Connect Pod to Athena, Epic, eClinicalWorks, or custom systems to sync insurance data.
Secure, HIPAA-compliant workflows
All data is encrypted and handled per HIPAA and regional privacy requirements—built for US healthcare providers.